In medicine, a chest radiograph, colloquially called a chest X-ray (CXR), or chest film, is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are among the most common films taken, being diagnostic of many conditions.
Like all methods of radiography, chest radiography employs ionizing radiation in the form of X-rays to generate images of the chest. The mean radiation dose to an adult from a chest radiograph is around 0.02 mSv (2 mrem) for a front view (PA or posterior-anterior) and 0.08 mSv (8 mrem) for a side view (LL or latero-lateral).
Problems identified

Chest radiographs are used to diagnose many conditions involving the chest wall, including its bones, and also structures contained within the thoracic cavity including the lungs, heart, and great vessels. Pneumonia and congestive heart failure are very commonly diagnosed by chest radiograph. Chest radiographs are used to screen for job-related lung disease in industries such as mining where workers are exposed to dust.
For some conditions of the chest, radiography is good for screening but poor for diagnosis. When a condition is suspected based on chest radiography, additional imaging of the chest can be obtained to definitively diagnose the condition or to provide evidence in favor of the diagnosis suggested by initial chest radiography. Unless a fractured rib is suspected of being displaced, and therefore likely to cause damage to the lungs and other tissue structures, x-ray of the chest is not necessary as it will not alter patient management.
The main regions where a chest X-ray may identify problems may be summarized as ABCDEF by their first letters:
- Airways, including hilar adenopathy or enlargement
- Breast shadows
- Bones, e.g. rib fractures and lytic bone lesions
- Cardiac silhoutte, detecting cardiac enlargement
- Costophrenic angles, including pleural effusions
- Diaphragm, e.g. evidence of free air, indicative of perforation of an abdominal viscus
- Edges, e.g. apices for fibrosis, pneumothorax, pleural thickening or plaques
- Extrathoracic tissues
- Fields (lung parenchyma), being evidence of alveolar flooding
- Failure, e.g. alveolar air space disease with prominent vascularity with or without pleural effusions
Views
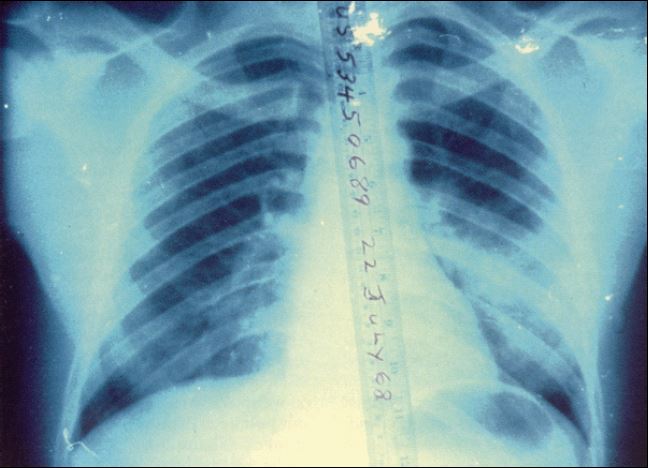
Different views (also known as projections) of the chest can be obtained by changing the relative orientation of the body and the direction of the x-ray beam. The most common views are posteroanterior, anteroposterior, and lateral. In an posteroanterior (PA) view, the x-ray source is positioned so that the x-ray beam enters through the posterior (back) aspect of the chest, and exits out of the anterior (front) aspect where the beam is detected. To obtain this view, the patient stands facing a flat surface behind which is an x-ray detector. A radiation source is positioned behind the patient at a standard distance (most often 6 feet, 1,8m), and the x-ray beam is fired toward the patient.
In anteroposterior (AP) views, the positions of the x-ray source and detector are reversed: the x-ray beam enters through the anterior aspect and exits through the posterior aspect of the chest. AP chest x-rays are harder to read than PA x-rays and are therefore generally reserved for situations where it is difficult for the patient to get an ordinary chest x-ray, such as when the patient is bedridden. In this situation, mobile X-ray equipment is used to obtain a lying down chest x-ray (known as a "supine film"). As a result, most supine films are also AP.
Lateral views of the chest are obtained in a similar fashion as the posteroanterior views, except in the lateral view, the patient stands with both arms raised and the left side of the chest pressed against a flat surface.
Typical views
Required projections can vary by country and hospital, typically an erect postero-anterior projection is first preference, if this is not possible then an antero-posterior view will be taken. Further imaging depends on local protocols which is dependent on the hospital protocols, the availability of other imaging modalities and the preference of the image interpreter.
Additional views
- Decubitus - taken while the patient is lying down, typically on his side. useful for differentiating pleural effusions from consolidation (e.g. pneumonia) and loculated effusions from free fluid in the pleural space. In effusions, the fluid layers out (by comparison to an up-right view, when it often accumulates in the costophrenic angles).
- Lordotic view - used to visualize the apex of the lung, to pick up abnormalities such as a Pancoast tumour.
- Expiratory view - helpful for the diagnosis of pneumothorax.
- Oblique view - useful for the visualization of the ribs and sternum. Although it's necessary to do the appropriate adaptations to the x-ray dosage to be used.
Abnormalities

Nodule
A nodule is a discrete opacity in the lung which may be caused by:
- Neoplasm: benign or malignant
- Granuloma: tuberculosis
- Infection: roundish pneumonia
- Vascular: infarct, varix, Wegener's granulomatosis, rheumatoid arthritis
There are a number of features that are helpful in suggesting the diagnosis:
- rate of growth
- Doubling time of less than one month: sarcoma/infection/infarction/vascular
- Doubling time of six to 18 months: benign tumour/malignant granuloma
- Doubling time of more than 24 months: benign nodule neoplasm
- calcification
- margin
- smooth
- lobulated
- presence of a corona radiata
- shape
- site
If the nodules are multiple, the differential is then smaller:
- infection: tuberculosis, fungal infection, septic emboli
- neoplasm: e.g., metastases, lymphoma, hamartoma
- sarcoidosis
- alveolitis
- auto-immune disease: e.g., Wegener's granulomatosis, rheumatoid arthritis
- inhalation (e.g., pneumoconiosis)
Cavities
A cavity is a walled hollow structure within the lungs. Diagnosis is aided by noting:
- wall thickness
- wall outline
- changes in the surrounding lung
The causes include:
- cancer
- infarct (usually from a pulmonary embolus)
- infection: e.g., Staphylococcus aureus, tuberculosis, Gram negative bacteria (especially Klebsiella pneumoniae), anaerobic bacteria, and fungus
- Wegener's granulomatosis
Pleural abnormalities
Fluid in space between the lung and the chest wall is termed a pleural effusion. There needs to be at least 75ml of pleural fluid in order to blunt the costophrenic angle on the lateral chest radiograph, and 200ml on the posteroanterior chest radiograph. On a lateral decubitus, amounts as small as 50ml of fluid are possible. Pleural effusions typically have a meniscus visible on an erect chest radiograph, but loculated effusions (as occur with an empyema) may have a lenticular shape (the fluid making an obtuse angle with the chest wall).
Pleural thickening may cause blunting of the costophrenic angle, but is distinguished from pleural fluid by the fact that it occurs as a linear shadow ascending vertically and clinging to the ribs.
Diffuse shadowing
The differential for diffuse shadowing is very broad and can defeat even the most experienced radiologist. It is seldom possible to reach a diagnosis on the basis of the chest radiograph alone: high-resolution CT of the chest is usually required and sometimes a lung biopsy. The following features should be noted:
- type of shadowing (lines, dots or rings)
- reticular (crisscrossing lines)
- companion shadow (lines paralleling bony landmarks)
- nodular (lots of small dots)
- rings or cysts
- ground glass
- consolidation (diffuse opacity with air bronchograms)
- location (where is the lesion worst?)
- upper (e.g., sarcoid, tuberculosis, silicosis/pneumoconiosis, ankylosing spondylitis, Langerhans cell histiocytosis)
- lower (e.g., cryptogenic fibrosing alveolitis, connective tissue disease, asbestosis, drug reactions)
- central (e.g., pulmonary edema, alveolar proteinosis, lymphoma, Kaposi's sarcoma, PCP)
- peripheral (e.g., cryptogenic fibrosing alveolitis, connective tissue disease, chronic eosinophilic pneumonia, bronchiolitis obliterans organizing pneumonia)
- lung volume
- increased (e.g., Langerhans cell histiocytosis, lymphangioleiomyomatosis, cystic fibrosis, allergic bronchopulmonary aspergillosis)
- decreased (e.g., fibrotic lung disease, chronic sarcoidosis, chronic extrinsic allergic alveolitis)
Pleural effusions may occur with cancer, sarcoid, connective tissue diseases and lymphangioleiomyomatosis. The presence of a pleural effusion argues against pneumocystis pneumonia.
- Reticular (linear) pattern
- (sometimes called "reticulonodular" because of the appearance of nodules at the intersection of the lines, even though there are no true nodules present)
- idiopathic pulmonary fibrosis
- connective tissue disease
- sarcoidosis
- radiation fibrosis
- asbestosis
- lymphangitis carcinomatosa
- PCP
- Nodular pattern
-
- sarcoidosis
- silicosis/pneumoconiosis
- extrinsic allergic alveolitis
- Langerhans cell histiocytosis
- lymphangitis carcinomatosa
- miliary tuberculosis
- metastases
- Cystic
-
- cryptogenic fibrosing alveolitis (late stage "honeycomb lung")
- cystic bronchiectasis
- Langerhans cell histiocytosis
- lymphangioleiomyomatosis
- Ground glass
-
- extrinsic allergic alveolitis
- diffuse interstitial pneumonitis
- alveolar proteinosis
- infant respiratory distress syndrome (RDS)
- Consolidation
-
- pneumonia
- alveolar haemorrhage
- alveolar cell carcinoma
- vasculitis
Signs
-
- The silhouette sign is especially helpful in localizing lung lesions. (e.g., loss of right heart border in right middle lobe pneumonia),
- The air bronchogram sign, where branching radiolucent columns of air corresponding to bronchi is seen, usually indicates air-space (alveolar) disease, as from blood, pus, mucus, cells, protein surrounding the air bronchograms. This is seen in Respiratory distress syndrome
- The "bean" sign first described by Professor Keval Pandya is the appearance of a sharply circumscribed bean shaped nodule on chest X-ray which has a high sensitivity and specificity (92% and 88%) for the presence of miliary TB.
Limitations
While chest radiographs are a cheap and relatively safe method of investigating diseases of the chest, there are a number of serious chest conditions that may be associated with a normal chest radiograph and other means of assessment may be necessary to make the diagnosis. For example, a patient with an acute myocardial infarction may have a completely normal chest radiograph.
Gallery
See also
- Abdominal x-ray
- Magnetic resonance imaging
- X-ray computed tomography
References
External links
- How to read a chest x-ray video by Pauley Chea, MD
- Chest X-ray Atlas
- USUHS: Basic Chest X-Ray Review
- eMedicine Radiology: Chest articles
- Database of chest radiology related to emergency medicine
- Introduction to chest radiology: a tutorial for learning to read a chest x-ray
- Chest Radiology Tutorials Free Web Tutorials for Chest Anatomy and Lung Malignancies in Radiology
- Yale: Introduction to Cardiothoracic Imaging




0 komentar :
Posting Komentar