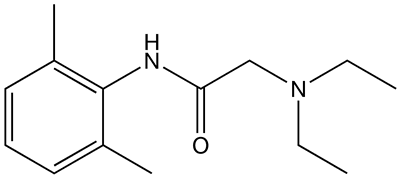
Lidocaine (INN, BAN) /ˈlaɪdɵkeɪn/, xylocaine, or lignocaine (AAN, former BAN) /ˈlɪɡnɵkeɪn/ is a common local anesthetic and class-1b antiarrhythmic drug. Lidocaine is used topically to relieve itching, burning, and pain from skin inflammations, injected as a dental anesthetic, or used as a local anesthetic for minor surgery.
It is on the WHO Model List of Essential Medicines, the most important medications needed in a basic healthcare system.
Medical uses
The efficacy profile of lidocaine as a local anesthetic is characterized by a rapid onset of action and intermediate duration of efficacy. Therefore, lidocaine is suitable for infiltration, block, and surface anesthesia. Longer-acting substances such as bupivacaine are sometimes given preference for subdural and epidural anesthesias; lidocaine, though, has the advantage of a rapid onset of action. Epinephrine (adrenaline) vasoconstricts arteries, reducing bleeding and also delays the resorption of lidocaine, almost doubling the duration of anaesthesia. For surface anesthesia, several available formulations can be used for endoscopies, before intubations, etc. Buffering the pH of lidocaine makes local freezing less painful. Lidocaine drops can be used on the eyes for short ophthalmic procedures.
Topical lidocaine has been shown in some patients to relieve the pain of postherpetic neuralgia (a complication of shingles), though not enough study evidence exists to recommend it as a first-line treatment. Intravenous lidocaine also has uses as a temporary fix for tinnitus. Although not completely curing the disorder, it has been shown to reduce the effects by around two-thirds.
Lidocaine is also the most important class-1b antiarrhythmic drug; it is used intravenously for the treatment of ventricular arrhythmias (for acute myocardial infarction, digoxin poisoning, cardioversion, or cardiac catheterization) if amiodarone is not available or contraindicated. Lidocaine should be given for this indication after defibrillation, CPR, and vasopressors have been initiated. A routine prophylactic administration is no longer recommended for acute cardiac infarction; the overall benefit of this measure is not convincing.
Inhaled lidocaine can be used as an antitussive (cough suppressor) acting peripherally to reduce the cough reflex. This application can be implemented as a safety and comfort measure for patients who have to be intubated, as it reduces the incidence of coughing and any tracheal damage it might cause when emerging from anesthesia.
Lidocaine, along with ethanol, ammonia, and acetic acid, has also been proven to be effective in treating jellyfish stings, both numbing the affected area and preventing further nematocyst discharge.
Insensitivity
Relative insensitivity to lidocaine is genetic. In hypokalemic sensory overstimulation, relative insensitivity to lidocaine has been described in people who also have attention deficit hyperactivity disorder. In dental anesthesia, a relative insensitivity to lidocaine can occur for anatomical reasons due to unexpected positions of nerves. Some people with Ehlers-Danlos syndrome are insensitive to lidocaine.
Contraindications
Absolute contraindications for the use of lidocaine include:
- Heart block, second or third degree (without pacemaker)
- Severe sinoatrial block (without pacemaker)
- Serious adverse drug reaction to lidocaine or amide local anesthetics
- Hypersensitivity to corn and corn-related products (corn-derived dextrose is used in the mixed injections)
- Concurrent treatment with quinidine, flecainide, disopyramide, procainamide (class I antiarrhythmic agents)
- Prior use of amiodarone hydrochloride
- Adams-Stokes syndrome
- Wolff-Parkinson-White syndrome
- Lidocaine viscous is not recommended by the FDA to treat tooth pain in children and infants.
Exercise caution in patients with any of these:
- Hypotension not due to arrhythmia
- Bradycardia
- Accelerated idioventricular rhythm
- Elderly patients
- Pseudocholinesterase deficiency
- Intra-articular infusion (this is not an approved indication and can cause chondrolysis)
- Porphyria, especially acute intermittent porphyria; lidocaine has been classified as porphyrogenic because of the hepatic enzymes it induces, although clinical evidence suggests it is not. Bupivacaine is a safe alternative in this case.
- Impaired liver function - people with lowered hepatic function may have an adverse reaction with repeated administration of lidocaine because the drug is metabolized by the liver. Adverse reactions may include neurological symptoms (e.g. dizziness, nausea, muscle twitches, vomiting, or seizures).
Adverse effects

Adverse drug reactions (ADRs) are rare when lidocaine is used as a local anesthetic and is administered correctly. Most ADRs associated with lidocaine for anesthesia relate to administration technique (resulting in systemic exposure) or pharmacological effects of anesthesia, and allergic reactions only rarely occur. Systemic exposure to excessive quantities of lidocaine mainly result in central nervous system (CNS) and cardiovascular effects â€" CNS effects usually occur at lower blood plasma concentrations and additional cardiovascular effects present at higher concentrations, though cardiovascular collapse may also occur with low concentrations. ADRs by system are:
- CNS excitation: nervousness, agitation, anxiety, apprehension, tingling around the mouth (circumoral paraesthesia), headache, hyperesthesia, tremor, dizziness, pupillary changes, psychosis, euphoria, hallucinations, and seizures
- CNS depression with increasingly heavier exposure: drowsiness, lethargy, slurred speech, hypoesthesia, confusion, disorientation, loss of consciousness, respiratory depression and apnoea.
- Cardiovascular: hypotension, bradycardia, arrhythmias, flushing, venous insufficiency, increased defibrillator threshold, edema, and/or cardiac arrest â€" some of which may be due to hypoxemia secondary to respiratory depression.
- Respiratory: Bronchospasm, dyspnea, respiratory depression or arrest
- Gastrointestinal: metallic taste, nausea, vomiting
- Ears: tinnitus
- Eyes: local burning, Conjunctival hyperemia, corneal epithelial changes/ulceration, diplopia, visual changes (opacification)
- Skin: itching, depigmentation, rash, urticaria, edema, angioedema, bruising, inflammation of the vein at the injection site, irritation of the skin when applied topically
- Blood: methemoglobinemia
- Allergy
ADRs associated with the use of intravenous lidocaine are similar to toxic effects from systemic exposure above. These are dose-related and more frequent at high infusion rates (≥3 mg/min). Common ADRs include: headache, dizziness, drowsiness, confusion, visual disturbances, tinnitus, tremor, and/or paraesthesia. Infrequent ADRs associated with the use of lidocaine include: hypotension, bradycardia, arrhythmias, cardiac arrest, muscle twitching, seizures, coma, and/or respiratory depression.
It is generally safe to use lidocaine with vasoconstrictor such as epinephrine including in regions such as the nose, ears, fingers and toes. While concerns of tissue death if used in these areas have been raised evidence does not support these concerns.
Overdosage
Overdoses with lidocaine can be a result of excessive administration by topical or parenteral routes, accidental oral ingestion of topical preparations by children who are more susceptible to overdose, accidental intravenous (rather than subcutaneous, intrathecal, or paracervical) injection, or prolonged use of subcutaneous infiltration anesthesia during cosmetic surgical procedures. These occurrences have often led to severe toxicity or death in both children and adults. Lidocaine and its two major metabolites may be quantified in blood, plasma, or serum to confirm the diagnosis in potential poisoning victims or to assist in the forensic investigation in a case of fatal overdose. It is important in the interpretation of analytical results to recognize that lidocaine is often routinely administered intravenously as an antiarrhythmic agent in critical cardiac-care situations. Treatment with intravenous lipid emulsions (used for parental feeding) to reverse the effects of local anaesthetic toxicity is becoming more commonplace.
Interactions
Any drugs that are also ligands of CYP3A4 and CYP1A2 can potentially increase serum levels and potential for toxicity or decrease serum levels and the efficacy, depending on whether they induce or inhibit the enzymes, respectively. Drugs that may increase the chance of methemoglobinemia should also be considered carefully. Dronedarone and liposomal morphine are both absolutely contraindicated, as they may increase the serum levels, but hundreds of other drugs require monitoring for interaction.
Dosage forms
Lidocaine, usually in the form of lidocaine hydrochloride, is available in various forms including:
- Injected local anesthetic (sometimes combined with epinephrine to reduce bleeding)
- Dermal patch (sometimes combined with prilocaine)
- Intravenous injection
- Intravenous infusion
- Intraosseous infusion
- Nasal instillation/spray (combined with phenylephrine)
- Oral gel (often referred to as "viscous lidocaine" or abbreviated "lidocaine visc" or "lidocaine HCl visc" in pharmacology; used as teething gel)
- Oral liquid
- Oral and topical ointments, with and without flavoring, respectively
- Topical gel (as with aloe vera gels that include lidocaine)
- Topical liquid
- Lidocaine HCl 2% jelly, combined with hypromellose, to anesthetize and lubricate the urethra, etc., for inserting a catheter or instrument
- Topical patch (lidocaine 5%), marketed since 1999 in the US by Endo Pharmaceuticals as "Lidoderm" - and since 2007 in the UK by Grünenthal as "Versatis"
- Topical ointment (lidocaine 5%) as a temporary reliever of discomfort associated anorectal disorders, such as hemorrhoids, marketed as an over-the-counter product in the US as RectiCare since 2012 by Ferndale Healthcare, Inc
- Topical aerosol spray
- Inhaled by nebulizer
- As a component of a GI cocktail used in emergency rooms
- Ophthalmic solution
Adulterant in cocaine
Lidocaine is often added to cocaine as a diluent. Cocaine numbs the gums when applied, and since lidocaine causes stronger numbness, a user gets the impression of high-quality cocaine when in actuality, the user is receiving a diluted product.
Preparation
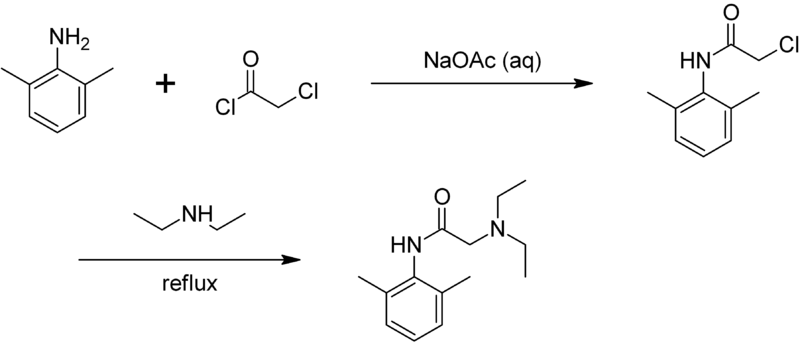
Lidocaine may be prepared in two steps by the reaction of 2,6-xylidine with chloroacetyl chloride, followed by the reaction with diethylamine:
Pharmacokinetics
The onset of action of lidocaine is about 45 to 90 sec and its duration is 10 to 20 min. It is about 95% metabolized (dealkylated) in the liver mainly by CYP3A4 to the pharmacologically active metabolites monoethylglycinexylidide (MEGX) and then subsequently to the inactive glycine xylidide. MEGX has a longer half-life than lidocaine, but also is a less potent sodium channel blocker. The volume of distribution is 1.1-2.1 l/kg, but congestive heart failure can decrease it. About 60-80% circulates bound to the protein alpha1 acid glycoprotein. The oral bioavailability is 35% and the topical bioavailability is 3%.
The elimination half-life of lidocaine is biphasic and around 90â€"120 min in most patients. This may be prolonged in patients with hepatic impairment (average 343 min) or congestive heart failure (average 136 min). Lidocaine is excreted in the urine (90% as metabolites and 10% as unchanged drug).
Pharmacodynamics
Anaesthesia
Lidocaine alters signal conduction in neurons by blocking the fast voltage-gated Na+ channels in the neuronal cell membrane responsible for signal propagation. With sufficient blockage, the membrane of the postsynaptic neuron will not depolarize and will thus fail to transmit an action potential. This creates the anaesthetic effect by not merely preventing pain signals from propagating to the brain, but by stopping them before they begin. Careful titration allows for a high degree of selectivity in the blockage of sensory neurons, whereas higher concentrations also affect other modalities of neuron signaling.
Antiarrhythmic
The same principle applies for this drug's actions in the heart. Blocking sodium channels in the conduction system, as well as the muscle cells of the heart, raises the depolarization threshold, making the heart less likely to initiate or conduct early action potentials that may cause an arrhythmia.
History
Lidocaine, the first amino amideâ€"type local anesthetic, was first synthesized under the name 'xylocaine' by Swedish chemist Nils Löfgren in 1943. His colleague Bengt Lundqvist performed the first injection anesthesia experiments on himself. It was first marketed in 1949.
Recreational use
Lidocaine is not currently listed by the World Anti-Doping Agency as an illegal substance. It is used as an adjuvant, adulterant, and diluent to street drugs such as cocaine and heroin.
Compendial status
- Japanese Pharmacopoeia 15
- United States Pharmacopeia 31
See also
- Lidocaine/prilocaine
- Dimethocaine (has some DRI activity)
- Procaine
References
External links
- U.S. National Library of Medicine: Drug Information Portal - Lidocaine
- Endo Pharmaceuticals' Lidoderm website




0 komentar :
Posting Komentar